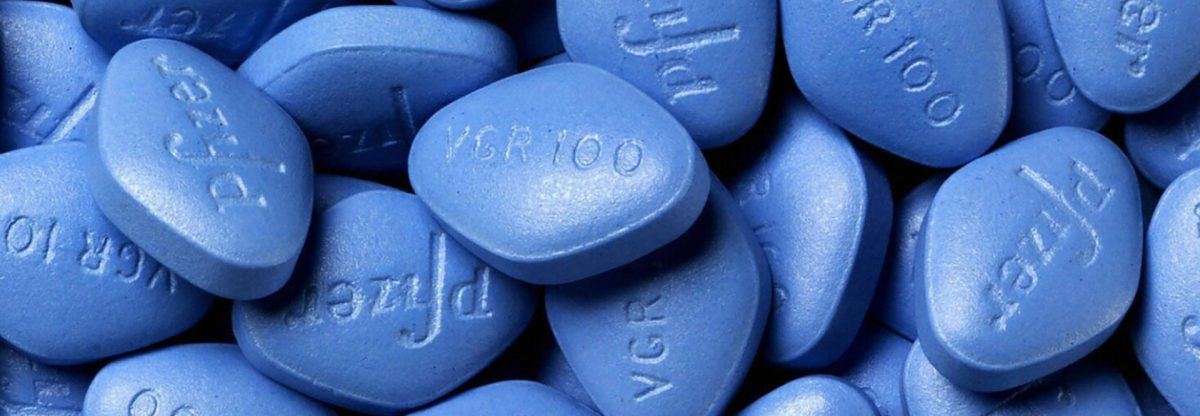
Cleveland Clinic research identifies sildenafil as a candidate drug for Alzheimer’s disease.
Findings published in Nature Aging show 69% reduced likelihood of developing the disease.
A new Cleveland Clinic-led study has identified sildenafil – an FDA-approved therapy for erectile dysfunction (Viagra) and pulmonary hypertension (Ravatio) – as a promising drug candidate to help prevent and treat Alzheimer’s disease.
According to findings published in Nature Aging, the research team, led by Feixiong Cheng, Ph.D., of Cleveland Clinic’s Genomic Medicine Institute, used computational methodology to screen and validate FDA-approved drugs as potential therapies for Alzheimer’s disease. Through a large-scale analysis of a database of more than 7 million patients, they determined that sildenafil is associated with 69% reduced incidence of Alzheimer’s disease, indicating the need for follow-up clinical trial testing of the drug’s efficacy in patients with the disease.
“Recent studies show that the interplay between amyloid and tau is a greater contributor to Alzheimer’s than either by itself,” said Dr. Cheng. “Therefore, we hypothesized that drugs targeting the molecular network intersection of amyloid and tau endophenotypes should have the greatest potential for success.”
Without the development of effective new treatments, Alzheimer’s disease is set to impact 13.8 million Americans by 2050, underscoring the need for rapid development of prevention and treatment strategies. Drug repurposing – use of an existing drug for new therapeutic purposes – offers a practical alternative to the costly and time-consuming traditional drug discovery process.
“This paper is an example of a growing area of research in precision medicine where big data is key to connecting the dots between existing drugs and a complex disease like Alzheimer’s,” said Jean Yuan, M.D., Ph.D., program director of Translational Bioinformatics and Drug Development at the National Institute on Aging (NIA), part of the National Institutes of Health (NIH), which funded this research. “This is one of many efforts we are supporting to find existing drugs or available safe compounds for other conditions that would be good candidates for Alzheimer’s disease clinical trials.”
Dr. Cheng’s team has found that understanding subtypes (endophenotypes) of neurodegenerative diseases such as Alzheimer’s disease may help to reveal common underlying mechanisms and lead to discovery of actionable targets for drug repurposing.
The buildup of beta amyloid and tau proteins in the brain leads to amyloid plaques and tau neurofibrillary tangles – two hallmarks of Alzheimer’s-related brain changes. The amount and location of these proteins in the brain may help define endophenotypes. However, no FDA-approved, anti-amyloid or anti-tau small molecule Alzheimer’s treatments currently exist, with many clinical trials for such treatments having failed in the past decade.
“Recent studies show that the interplay between amyloid and tau is a greater contributor to Alzheimer’s than either by itself,” said Dr. Cheng. “Therefore, we hypothesized that drugs targeting the molecular network intersection of amyloid and tau endophenotypes should have the greatest potential for success.”
Using a large gene-mapping network, researchers integrated genetic and other biologic data to determine which of over 1,600 FDA-approved drugs could be an effective treatment for Alzheimer’s disease. They pinpointed drugs that target both amyloid and tau as having higher scores compared to drugs that target just one or the other. “Sildenafil, which has been shown to significantly improve cognition and memory in preclinical models, presented as the best drug candidate,” said Dr. Cheng.
The research team utilized a large database of claims data of more than 7 million people in the U.S. to examine the relationship between sildenafil and Alzheimer’s disease outcomes by comparing sildenafil users to non-users. The analysis included patients using comparator drugs that either were in an active Alzheimer’s clinical trial (losartan or metformin) or were not yet reported as relevant to the disease (diltiazem or glimepiride).
They found that sildenafil users were 69% less likely to develop Alzheimer’s disease than non-sildenafil users after 6 years of follow-up. Specifically, sildenafil had a 55% reduced risk of the disease compared to losartan, 63% compared to metformin, 65% compared to diltiazem and 64% compared to glimepiride.
“Notably, we found that sildenafil use reduced the likelihood of Alzheimer’s in individuals with coronary artery disease, hypertension, and type 2 diabetes, all of which are comorbidities significantly associated with risk of the disease, as well as in those without,” added Dr. Cheng.
To further explore sildenafil’s effect on Alzheimer’s disease, the researchers developed an Alzheimer’s patient-derived brain cell model using stem cells. In the model, they found that sildenafil increased brain cell growth and decreased hyperphosphorylation of tau proteins (a hallmark that leads to neurofibrillary tangles), offering biological insights into how sildenafil may influence disease-related brain changes.
“Because our findings only establish an association between sildenafil use and reduced incidence of Alzheimer’s disease, we are now planning a mechanistic trial and a phase II randomized clinical trial to test causality and confirm sildenafil’s clinical benefits for Alzheimer’s patients,” said Dr. Cheng. “We also foresee our approach being applied to other neurodegenerative diseases, including Parkinson’s disease and amyotrophic lateral sclerosis, to accelerate the drug discovery process.”
Reference: “Endophenotype-based in silico network medicine discovery combined with insurance record data mining identifies sildenafil as a candidate drug for Alzheimer’s disease” 6 December 2021, Nature Aging.
DOI: 10.1038/s43587-021-00138-z
Jiansong Fang, Ph.D., a former research scholar in Dr. Cheng’s lab; Pengyue Zhang, Ph.D., an assistant research professor at Indiana University School of Medicine; Yadi Zhou, Ph.D., a data scientist in Dr. Cheng’s lab; and Chien-Wei Chiang, Ph.D., a research scientist at The Ohio State University College of Medicine, are co-first authors. Dr. Cheng presented the initial findings at the 2021 Alzheimer’s Association International Conference. The study was supported by NIA, NIH grants R01AG066707 and R01AG066707-01S1, and the Translational Therapeutics Core of the Cleveland Alzheimer’s Disease Research Center.